Medisin og helse Corona
- Trådstarter Disqutabel
- Startdato
Diskusjonstråd Se tråd i gallerivisning
-
Z
Zomby_Woof
Gjest
Sett på Rema i dag:
Tre damer med engstelig kroppsspråk og skjerf foran ansiktet. Tror ikke det hjelper å være redd. Tror ikke det hjelper mye å ha et ullskjerf foran ansiktet. Tror kanskje det virker mot sin hensikt ettersom de alle tre gjentatte ganger strammet, rettet, og holdt i skjerfet med de samme fingrene de fylte handlekurvene med. Det så til og med ut som en av dem på et tidspunkt rett og slett beit i skjerfet for å holde det på plass.
Håper virkelig ikke toskeskap er så smittsomt som man av og til kan tro...Når du bruker argumentet jeg kjeder meg til grensevaktene da du burde gi full support til handelsstand her hjemme da er du intet mindre enn

https://www.nrk.no/osloogviken/mange-nordmenn-i-karantene-etter-_harry-handel_-1.14978233GGjestemedlem
Gjest
Presis, spesielt med tanke på at dråpesmitte med kontakt er viktigere enn via luft... der er en grunn at at ikke den lille rakkeren får deg til å nyse. De fleste kunne like gjerne knytt tekstilet rundt anklene.Sett på Rema i dag:
Tre damer med engstelig kroppsspråk og skjerf foran ansiktet. Tror ikke det hjelper å være redd. Tror ikke det hjelper mye å ha et ullskjerf foran ansiktet. Tror kanskje det virker mot sin hensikt ettersom de alle tre gjentatte ganger strammet, rettet, og holdt i skjerfet med de samme fingrene de fylte handlekurvene med. Det så til og med ut som en av dem på et tidspunkt rett og slett beit i skjerfet for å holde det på plass.
Håper virkelig ikke toskeskap er så smittsomt som man av og til kan tro...GGjestemedlem
Gjest
Samme med korona, hadde det vært superdødelig ville det vært dødd ut for lenge siden siden ingen hadde overlevd lenge nok til å smitte noen andre.Toskeskap er det viruset som er mest aggresivt av alle - og som aldri forsvinner heller. MEN - dødeligheten er heldigvis lav. Kan være vanskelige å leve med...
Virus want to become you..
Det var vel strengt tatt Paul som fant ho?Jeg har jaggu meg funnet selveste dronningen av Corona
Hun heter Rosie. Er det pasient 0 tro?
Ja, men jeg oppdaget det 49 år etterpå
Det var vel strengt tatt Paul som fant ho?Jeg har jaggu meg funnet selveste dronningen av Corona
Hun heter Rosie. Er det pasient 0 tro?
Har måttet et par ærend de siste dagene og de aktuelle handlestedene er fulle av koronaidioter, vel en kan kanskje dele de i tre, proporsjonene er umulig å si noe om men om en tar utgangspunkt i:
1/3 ordentlige mennesker som gjør alt for unngå nærkontakt mv-
1/x del som ikke bryr seg så veldig mht ta hensyn, back to business.
1/Y del som hoster deg dett opp i ansiktet på vei ut av dagligvareforretningen...
Summasumarium jeg synes det er for stor andel som gir litt fn.
En kan jo spørre seg, er viruset mindre smittsomt nå? Eller...
Hva faen skjedde i startfasen av smittefasen? Gjorde folk alt de kunne for å bli sprayet/smittet og,
Utenom dette: Er dette et jævla kinesisk eksperiment som gikk lit ut av kontroll? Israelittene jobbet etter sigende med kjemiske våpen som kun skulle ta livet av arabere,
Sant!..
Well...,Om dette videoklippet er korrekt oppstod spanskesyken i en US*camp. Bør sees...
GGjestemedlem
Gjest
Tjo hei...
Om dette videoklippet er korrekt oppstod spanskesyken i en US*camp. Bør sees...
Det som er svært interessant med denne dokuen er at man konkluderer med at viruset «ran out of furl» dvs det hadde smittet alle som var mottagelige og spredningen stoppet opp av seg selv. Hadde det ikke det ville vel hele verdens befolkning vært utsletter.
Men er vi der nå? Er dette viruset og to run out of fuel?
Det antydes i filmen at 1918 viruset kan ha vært en etterlevning fra 1898 pandemien , som har ligger i dvale og bare ventet på de rette betingelser for å blomstre an so the story goes.
Se filmen, anbefales på det sterkeste.Israelittene jobbet etter sigende med kjemiske våpen som kun skulle ta livet av arabere,
Sant!..
Well...,
Det snakkes i visse etteretningskretser i den retning. At det var en liten overambisiøs kreativ gjeng som begynte et forskningsprosjekt for å finne et gen som var spesifikt for arabere som ikke jøder og vetslige hadde. Formålet skulle i følge de samme kilder ha vært å utvikle et genetisk våpen. Nå sier den samme historien også at de ikke fant noe slikt gen før det dukket opp "noen voksne" les: "ansvarlige politikere på høyt nivå" som stoppet prosjektet øyeblikkelig da fant ut hva som foregikk! Det sies at en berørt statsminister ble hylende forbannet og gav utvedtydig meldig om at jøder av alle folk, med den histroien de hadde bak seg, ALDRI skulle begynne å lage våpen for å utrydde folk på etnisk grunnlag! Rent offisiellt så skjedde ikke noe av dette,... aldri!
Noe tyder på at det heller ikke finnes noe skriftlig materiale som man en gang i framtiden kan risikere blir nedgradert, pussig!
Så historien er henvist til fortrolige samtaler i mørke kroker.
Det er det som er flokkimmunitet.Det som er svært interessant med denne dokuen er at man konkluderer med at viruset «ran out of furl» dvs det hadde smittet alle som var mottagelige og spredningen stoppet opp av seg selv. Hadde det ikke det ville vel hele verdens befolkning vært utsletter.
Men er vi der nå? Er dette viruset og to run out of fuel?
Trolig må 50-70% av befolkningen smittes for å oppnå det.
Dødeligheten er det stor usikkerhet rundt. Trolig ca 0,5% i land med god helsetjeneste og kanskje 1% der det ikke er det.
Så dette stopper nok ikke befolkningsveksten en gang.UUtgatt24668
Gjest
Med mørketall så tror jeg det ligger lavere enn 1% selv i utviklingsland. Covid-19 vil ikke helpe på overbefolkning nei..
Det er det som er flokkimmunitet.Det som er svært interessant med denne dokuen er at man konkluderer med at viruset «ran out of furl» dvs det hadde smittet alle som var mottagelige og spredningen stoppet opp av seg selv. Hadde det ikke det ville vel hele verdens befolkning vært utsletter.
Men er vi der nå? Er dette viruset og to run out of fuel?
Trolig må 50-70% av befolkningen smittes for å oppnå det.
Dødeligheten er det stor usikkerhet rundt. Trolig ca 0,5% i land med god helsetjeneste og kanskje 1% der det ikke er det.
Så dette stopper nok ikke befolkningsveksten en gang.Angående flokkimmunitet som noen har konkludert med skjer når tilstrekkelig mange nok har hatt sykdommen. Er fortsatt stor usikkerhet om dette virkelig skjer og i så fall hvor lenge man er immun. Det blir som professoren sa; Jeg vil ikke ha dette viruset i kroppen, det kødder med immunsystemet. Derfor burde vi holde dette så langt nede som det er mulig og vente på mer kunnskap.
https://www.dagbladet.no/nyheter/ble-syk-igjen-etter-fire-uker/72344786
Bl.a.
Om man blir immun for viruset etter å ha hatt sykdommen, er noe som forskes på, og spørsmålet er fortsatt veldig usikkert, sier assisterende helsedirektør Espen Nakstad i Helsedirektoratet til NRK.
Forskere i Shanghai har funnet overraskende lave nivåer av antistoffer hos pasienter som har gjennomgått covid-19-sykdommen, skriver South China Morning Post.
I alt er blodprøver fra 175 pasienter analysert, og i nær en tredel av dem er det svært lave nivåer av antistoffer. Hos enkelte fant forskerne ingen antistoffer overhodet.
- De fleste får nok en lang nok immunitet til at man får slått ned pandemier som denne, men det avhenger også av hvor stor endring det er i viruset, sa lege Harald Dobloug.
Edit.
Og det er denne taktikken svenskene kjører beinhardt på.
https://www.svt.se/nyheter/utrikes/appen-som-vill-oppna-upp-samhallet
Bl.a.
– Har man ett intyg på att man är immun så kan man ju gå tillbaka till jobbet eller umgås med vänner igen, säger Anders Jonson, projektledare för appen CoronaFree som inte spårar de som har corona – utan de som haft det, och blivit immuna
– Har man antikroppar så är det troligt att man inte får sjukdomen igen, i alla fall inte inom det närmaste året. Och om det blir så som man förutspår, att 60% av Sveriges befolkning kommer att ha smittats innan det här börjar avta ordentligt, så vill man ju naturligtvis veta om man själv tillhör de här 60 procenten eller är kvar i gruppen som fortfarande kan bli smittad, säger medicinska rådgivaren Gunnar Klein, professor i informatik och läkare som tidigare forskat i immunologi.Sist redigert:Forskere har enda ikke fastslått om det oppstår immunitet, noe som bør gi god grunn til ettertanke. I USA har man arrangert Coronavirusparties. Det er en dårlig ide syns denne epidemiologen, som lister opp noen grunner.
Greta Bauer er professor i epidemiologi og biostatistikk.
Hun er også innom de alvorlige følgeskadene, for hjerte og lunger.
www.nytimes.com/2020/04/08/opinion/coronavirus-parties-herd-immunity.html?
As the coronavirus continues to spread, epidemiologists like me are starting to field a remarkable question: Would people be better off if they just contracted the virus and got it over with? I’ve heard rumblings about people avoiding physical distancing or hosting a version of “chickenpox parties,” where noninfected people mingle with an infected person in an effort to catch the virus.
For some, it is part of a “herd immunity strategy” to build population immunity by infecting younger people who seem to have mild cases of Covid-19. Others are frustrated with staying home. There are also those who hope they could better protect their loved ones, serve their communities or return to work if they could develop immunity.
While frustration, fear and solution-seeking are normal responses to this new global risk, there are seven clear reasons choosing to get intentionally infected would be a really horrible idea right now.
It is all about how much we just don’t know yet.
1. Immunity isn’t a sure thing
We have not yet established that those who recover from this infection indeed develop long-term immunity. Herd immunity projections depend completely on such a sustained immune response, and we haven’t found out whether that even exists. We all sincerely hope it does, but we won’t know for certain until we study recovered patients over time.
2. Reinfection could be possible
There are documented cases where people who appear to recover from the virus test positive again, which calls even short-term immunity into question. These apparent cases of reinfection may actually be remission and relapse, or false test results. However, researchers need more time to figure out what is happening with these patients, and the implications.
What’s more, even if it is determined that reinfection cannot occur shortly after recovery, it could still happen later if immunity is only seasonal. If reinfection is indeed possible, we need to know whether it will result in disease that is milder or more severe. While antibodies to a previous infection generally reduce risk the second time around, for some viruses, such as dengue fever, they can lead to severe and even fatal disease.
3. The virus could continue living inside you
We don’t know that recovered patients actually clear the virus from their bodies. Many viruses can remain in reservoirs, parts of the body where they hang out quietly, and re-emerge to cause disease later in life. For example, chickenpox can come back as shingles, and hepatitis B can lead to liver cancer years later. We now know that in some patients, detectable virus can be found in feces and even blood after apparent recovery. Does the coronavirus remain in the body, or are these just residual bits of virus?
4. Even the young can be hospitalized
Hospital beds and equipment are urgently needed right now for Covid-19 patients. People shouldn’t kid themselves that because they are young they will not be hospitalized if infected. In the United States, the C.D.C. has estimated that about one in every five or six people aged 20 to 44 with confirmed Covid-19 has required hospitalization. Avoidable hospitalizations take valuable resources away from others who were not able to avoid infection.
5. Survivors could suffer long-term damage
While early reports focused almost exclusively on the risk of death, we do not yet fully understand the other effects of Covid-19. We do know that previously healthy people are being left with potentially long-term lung and heart damage.
6. A ‘mild’ case is hardly mild
As more patients recount enduring painful coughing, disorientation and difficulties breathing, people are coming to understand that the 80 percent to 85 percent of cases considered mild are not necessarily “mild” in its usual sense. Researchers and health care professionals use the term “mild” to describe Covid-19 cases not requiring hospitalization. While “mild” can be truly mild, it can also include pneumonia, and be brutal and scary.
7. There’s no shortcut to immunity
Herd immunity requires a high proportion of a population to be immune (the actual percentage varies for different infections), but we want to get there slowly or, ideally, through vaccines. Right now, too many people are getting sick through non-intentional spread, burdening hospitals and leading to severe illness and death. It is far too early to think about intentional infection as a strategy.
Slowing down the spread of the coronavirus won’t just save lives in the coming few months; it also gives us time to study treatments, and to expand or reconfigure hospital services for Covid-19 patients. This means that those who get sick later may benefit from better care, including effective medications. Of course, it also gives us more time to improve testing accuracy and capacity, and to develop a vaccine.
We need to keep in mind that the science is moving fast right now. It is unprecedented to see such an intensive effort internationally being put into studying one disease.
While it is hard to be patient, the best way out of this will likely be much clearer to us in a month or two than it is now. In the meantime, it is important that we don’t take unnecessary risks with unknown consequences. If we can avoid infection, we need to do exactly that.I motsatt retning; en artikkel som tyder på (kanskje?) at en god del personer kan ha en viss kryssimmunitet fra tidligere koronavirus, og at dette kan være en del av forklaringen på at enkelte ikke blir så veldig syke:
https://tidsskriftet.no/2020/04/kronikk/koronaviruset-kryssimmunitet-flokkimmunitet-og-vaksineutvikling
"En immunreaksjon mot et virusantigen gir opphav til hukommelses-B-celler, antistoffutskillende plasmaceller og hukommelses-T-celler. Slike celler og antistoff kan potensielt kryssreagere mot andre antigener. Dette kalles en immunologisk kryssreaksjon og gir kryssimmunitet mot smitte. I det følgende omtales først det nye og det forrige sarsviruset, reseptoren de benytter for opptak og et eksempel på kryssimmunitet. Deretter introduseres sesongkoronavirus som forårsaker luftveissykdom, og som kanskje kan være årsaken til en delvis beskyttelse i befolkningen. Til slutt forklares hvordan antistoff kan hjelpe covid-19-pasienter med alvorlig sykdom og hvorfor det er godt håp om en effektiv vaksine."
Igjen. nok et eksempel på at det skjer en enorm kunnskapsutvikling på dette området nå. I hvert fall er dette en hypotese som kan generere kunnskap med noe mer testing. Kan man for eksempel få en viss immunitet ved å først å smittes med mindre alvorlige coronavirus?fra Washington’s permanent influence industry
gode tider!
The coronavirus pandemic has gut-punched global markets, put 6.6 million Americans out of work and raised the likelihood of a recession. But in the Washington lobbying world, business is booming.
Companies, interest groups and entire industries are seeking help from lobbyists as they navigate a chaotic environment to secure a piece of the record $2.2 trillion financial aid package the Trump administration must quickly pump out in an effort to stabilize the U.S. economy.
https://apnews.com/fac2794db22630c0da51a20f8d588ca9
––––
and the winners are… sannsynligvis the usual suspectsJa, det med virusimmunitet har vel aldri vært svart hvitt. Jeg oppfatter det som en etablert sannhet folk som er godt oppe i årene gjennomgående har bedre virus-immunitet enn den yngre garde ... selv om disse virusene alltid er litt forskjellig fra forrige gang.LItt nyttig info.
Hvor er Lydia Pinkham når vi trenger hennes medicinal compound mer enn noensinne?
Man skal nok til å revurdere strategier. Dette viruset gir nye utfordringer.
I tillegg til studien fra Kina, der 1/3 av 175 testsubjekter ikke hadde antistoffer, mens de resterende hadde meget få, viser Sør-Korea nå til at 74 friskmeldte er blitt smittet påny.
NRK følger opp:
https://www.nrk.no/urix/nye-funn-reiser-tvil-om-immunitet-mot-korona-1.14977519

Nå er det du som grovregner.Det er det som er flokkimmunitet.
Trolig må 50-70% av befolkningen smittes for å oppnå det.
Flokkimmunitet er definert som at tilstrekkelig mange i populasjonen har etablert immunitet til at det effektive spredningstallet R dupper under 1,0 og smitten avtar. Hvor stor prosent av befolkningen kommer an på hvor smittsomt det er i utgangspunktet og kan anslås som 1-1/R. Dette viruset så ut til å ha R et sted rundt 2-2,5 da det først begynte å spre seg i Norge. Det tilsier ca 60 %, men det tilsier også at f..skapen sprer seg eksponensielt med doblingstid på ca en uke. En influensa med R = 1,3 vil gi seg når ca 25 % av befolkningen er smittet. Under betingelser som gir R = 5, som i tidlig fase av covid-19 i Kina, vil 80 % bli smittet før det "brenner ut".
Og hvis det viser seg å gi veldig begrenset immunitet, som noen studier kan tyde på, så vil det bare gå rundt og rundt som enslags periodisk utsortering av gamle og andre med underliggende sykdommer, omtrent som en ulveflokk rydder i en elgbestand. Vi bør kanskje være litt forbi denslags. Da kan viruset beskrives som endemisk, R = 1,0, og antall syke vil være omtrent konstant over lang tid.
Hvis vi blander begrepene litt kan vi hevde at Norge nå har en adferdsbasert "flokkimmunitet", ettersom sosial distansering og intens håndvask har ført til R = 0,7 eller deromkring. Det funker også, så lenge flokken oppfører seg.Sist redigert:Like mange døde i Sverige på en dag som det er totalt døde i Norge (105).
Like fullt en litt oppløftende artikkel i VG i dag (bak betalingsmur).
https://www.vg.no/forbruker/helse/i/8m8PX1/forskere-coronaviruset-muterer-slik-utvikles-det-naa
Hvis det er rett det som skrives om at det er sterkt begrenset immunitet etter sykdom, og at viruset muterer til en mindre farlig variant (som artikkelen i vg også hinter om) er Sveriges strategi absolutt ikke å anbefale.Sist redigert:Sverige har vel nå ca 8 ganger så mange døde som Norge, forrige uke var det 6, uka før det 3
(Hvis jeg husker riktig, ukene begynner gli inn i hverandre her nå. 3-6-8 utvikling har vært der ihvertfall)
En faktor her er at man ved et vanlig forløp får flere og flere i befolkningen som er immune. Virus finner det dermed vanskelig å komme videre fra en vert, siden nye og potensielle verter ikke er mottakelige for å hjelpe viruset med å replisere seg, siden viruset ikke får igangsatt de nødvendige mekanismene. Dette er også poenget med vaksiner (og årsaken til at man bør forsøke å omvende vaksinemotstandere). Man reduserer antallet overførere av en infeksjon.
Nå er det du som grovregner.Det er det som er flokkimmunitet.
Trolig må 50-70% av befolkningen smittes for å oppnå det.
Flokkimmunitet er definert som at tilstrekkelig mange i populasjonen har etablert immunitet til at det effektive spredningstallet R dupper under 1,0 og smitten avtar. Hvor stor prosent av befolkningen kommer an på hvor smittsomt det er i utgangspunktet og kan anslås som 1-1/R. Dette viruset så ut til å ha R et sted rundt 2-2,5 da det først begynte å spre seg i Norge. Det tilsier ca 60 %, men det tilsier også at f..skapen sprer seg eksponensielt med doblingstid på ca en uke. En influensa med R = 1,3 vil gi seg når ca 25 % av befolkningen er smittet. Under betingelser som gir R = 5, som i tidlig fase av covid-19 i Kina, vil 80 % bli smittet før det "brenner ut".
Og hvis det viser seg å gi veldig begrenset immunitet, som noen studier kan tyde på, så vil det bare gå rundt og rundt som enslags periodisk utsortering av gamle og andre med underliggende sykdommer, omtrent som en ulveflokk rydder i en elgbestand. Vi bør kanskje være litt forbi denslags. Da kan viruset beskrives som endemisk, R = 1,0, og antall syke vil være omtrent konstant over lang tid.
Hvis vi blander begrepene litt kan vi hevde at Norge nå har en adferdsbasert "flokkimmunitet", ettersom sosial distansering og intens håndvask har ført til R = 0,7 eller deromkring. Det funker også, så lenge flokken oppfører seg.
Dersom sykdommen SARS-CoV-2 forårsaker ikke gjør oss immune betyr det at viruset ikke slipper opp for verter og som Asbjørn skriver vil det da "gå rundt og rundt" blant oss. Et problem er at det ikke bare fjerner dem med underliggende sykdommer, men at det skader yngre som overlever alvorlige infeksjoner (hjerte, nyre og lunger) og svekker disse med tanke på neste virusomgang.
Verden har hatt fra slutten av november til nå for å innhente erfaringer med dette viruset, så mye er uklart.
Vi er enig i formelen her, og 50% svarer til en R på 2 og 70% til en R på 3,3.
Nå er det du som grovregner.Det er det som er flokkimmunitet.
Trolig må 50-70% av befolkningen smittes for å oppnå det.
Flokkimmunitet er definert som at tilstrekkelig mange i populasjonen har etablert immunitet til at det effektive spredningstallet R dupper under 1,0 og smitten avtar. Hvor stor prosent av befolkningen kommer an på hvor smittsomt det er i utgangspunktet og kan anslås som 1-1/R. Dette viruset så ut til å ha R et sted rundt 2-2,5 da det først begynte å spre seg i Norge. Det tilsier ca 60 %, men det tilsier også at f..skapen sprer seg eksponensielt med doblingstid på ca en uke. En influensa med R = 1,3 vil gi seg når ca 25 % av befolkningen er smittet. Under betingelser som gir R = 5, som i tidlig fase av covid-19 i Kina, vil 80 % bli smittet før det "brenner ut".
Og hvis det viser seg å gi veldig begrenset immunitet, som noen studier kan tyde på, så vil det bare gå rundt og rundt som enslags periodisk utsortering av gamle og andre med underliggende sykdommer, omtrent som en ulveflokk rydder i en elgbestand. Vi bør kanskje være litt forbi denslags. Da kan viruset beskrives som endemisk, R = 1,0, og antall syke vil være omtrent konstant over lang tid.
Hvis vi blander begrepene litt kan vi hevde at Norge nå har en adferdsbasert "flokkimmunitet", ettersom sosial distansering og intens håndvask har ført til R = 0,7 eller deromkring. Det funker også, så lenge flokken oppfører seg.
Målet med flokkimmunitet er jo at vi kan fjerne alle smitteverntiltak uten at viruset blusser opp.
Med dagens smittevernstiltak har vi en R på ca 1.
Når et nå mykes opp litt, vil den nok komme over 1.
Hvis man gjør som svenskene og dette er et poeng som litt underkommuniserte i feks SSB sin rapport og også Helsedirektoratet sin rapport - så har man smittetiltak for å flate ut toppen. Men når man har passert toppen, så kan man lette på tiltakene - og da kan man lette de ganske raskt.
For å illustrere poenget - hvis skoler, butikker og det meste åpner opp igjen. Vi har fortsatt begrensninger på konserter/kino og noe begrensinger på større forsamlinger. Og vi oppfordrer fortsatt til hjemmekontor, smitteverntiltak i butikker osv. La oss si at det gir oss en R på 1,4. Med 25% av befolkningen immun så blir den effektive R 1,05.
Her er det også viktig at smitten sprer seg ikke likt i landet. Så mens man med feks 30 000 smittede på landsbasis er langt under 1% av "flokken", vil det kanskje være 10-20% av de i omgangskretsen til de som er smittet som er immune - så denne bremsen som følge av flokkimmunitet får man ganske tidlig.
Det kan godt tenkes at svenskene (og vi om vi følger en slikt strategi) må slå på bremsene et sted på vei oppover. Brems scenariet har en R på 1,3 - og for å unngå at man går over kapasitet - så kan det være fordelaktig og innføre strengere tiltak for presse R ned til 1.
Men, når man har kommet over toppen, så kan man ganske radig fjerne tiltakene - da flokkimmuniteten hele tiden vokser. Og på slutten så spiller det egentlig ikke den helt store rollen om R0 er 2, 3 eller 4. Det vil brenne ut til slutt.
Jeg skjønner det er interessant å debattere om viruset gir immunitet - men det jobber sikkert såpass mange i folkehelseinstituttet i ulike land som har denne strategien, at det er sikkert lurt å stole mer på de, enn noen enkelte artikler her og der.De folkehelseinstituttene leser nok de samme artiklene. Vi vet faktisk ikke ennå. Ingen vet dette sikkert. Man kan gjøre ulike antagelser og vurdere risiko litt ulikt, og det ser ut til at Sverige har gjort en litt annen vurdering enn stort sett alle andre sammenlignbare land. De risikerer å få høyere menneskelige kostnader og omtrent like høye økonomiske kostnader som nabolandene. Svensker flest følger myndighetenes råd, så adferden er ikke så ulik den man ser i Norge, unntatt i enkelte miljøer som vil bli «hot spots».
Jeg mener fortsatt at en strategi med sikte på å oppnå «flokkimmunitet», dvs la en stor prosentandel av befolkningen bli smittet, vil være en uakseptabel risiko. Vi vet ikke nok om eventuell immunitet, men vi vet allerede en hel del om både smittsomhet og dødelighet, og at en eksponensiell vekst selv med R = 1,3 eller deromkring ville sprenge intensivkapasiteten ganske fort.
Siste estimat jeg har sett er fortsatt R=0,71. Vi får se om det kravler oppover igjen, men påsken er normalt en ukes lockdown i Norge, så det kan godt hende at det fortsetter nedover til over påske og gradvis gjenåpning.Bedre grunn til å begynne å trene, spise mindre fett og sukker og å ta av noen kilo finner du aldri noensinne igjen. Diabetes og overvekt overrepresentert blant intensivpasienter. Antageligvis verre enn moderat røyking om man ellers er slank og i god form. Siste setning er min ukvalifiserte gjetting...
https://www.vg.no/nyheter/innenriks...rfor-blir-overvektige-sykere-av-coronavirusetDe folkehelseinstituttene leser nok de samme artiklene. Vi vet faktisk ikke ennå. Ingen vet dette sikkert. Man kan gjøre ulike antagelser og vurdere risiko litt ulikt, og det ser ut til at Sverige har gjort en litt annen vurdering enn stort sett alle andre sammenlignbare land.
https://www.fhi.no/contentassets/c9...bd0/notat-om-risiko-og-respons-2020-04-05.pdf
I følge denne så har vel både Sverige, Danmark, Nederland, Storbritannia valg Brems.
Jeg følger meg trygg på at fagmiljøene i disse landene er såpass sterke at de har gjort en vurdering rundt flokkimmunitet.
Jeg ser det du til stadighet nevner eksponensiell vekst med 1,3 kan sprenge kapasiteten (Jeg er selvsagt enig i at en kurve som vokser med en faktor på 1,3 hver uke til slutt vil overstige kapasteten, men jeg mener jo at denne R faktoren kan justeres og vil bli påvirket av flokkimmunitet underveis. Det ser vi vel litt i Sverige.
Mener du at denne strategien ikke åpner for å innføre strengere tiltak underveis dersom belastningen nærmer seg maks, eller mener du at vi ikke greier å få ned R til 1 eller under - hvis vi først har sluppet det opp så mye..?
Nå er nok diabetes, hjerteproblemer og alle de andre problemer overvekt medfører mye farligere enn Corona for de aller fleste i denne kategorien.Bedre grunn til å begynne å trene, spise mindre fett og sukker og å ta av noen kilo finner du aldri noensinne igjen. Diabetes og overvekt overrepresentert blant intensivpasienter. Antageligvis verre enn moderat røyking om man ellers er slank og i god form.
https://www.vg.no/nyheter/innenriks...rfor-blir-overvektige-sykere-av-coronaviruset
Det før vel drøyt 3000 mennesker hvert år som følge av overvekt.
Jo, men risikoen er betraktelig høyere uansett andre farer. Det var bare det som var poenget mitt. At man kan dø av diverse tilstander med eller uten virusets eksistens er vel helt irrelevant.
Nå er nok diabetes, hjerteproblemer og alle de andre problemer overvekt medfører mye farligere enn Corona for de aller fleste i denne kategorien.Bedre grunn til å begynne å trene, spise mindre fett og sukker og å ta av noen kilo finner du aldri noensinne igjen. Diabetes og overvekt overrepresentert blant intensivpasienter. Antageligvis verre enn moderat røyking om man ellers er slank og i god form.
https://www.vg.no/nyheter/innenriks...rfor-blir-overvektige-sykere-av-coronaviruset
Det før vel drøyt 3000 mennesker hvert år som følge av overvekt.GGjestemedlem
Gjest
Tino Sanandaji
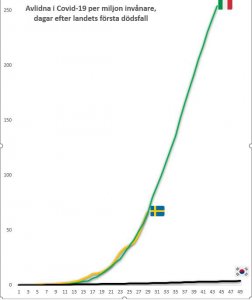
Idag kom spiken i kistan för Sveriges strategi när slumpmässiga tester i Stockholm visar att endast 2,5 procent var smittade vid testtillfälle, långt ifrån de ca 50 procent som krävs för självimmunisering genom flockimmunintet. Trots ständig försäkran att kurvan snart planar har vi ännu en dag när Sveriges rapporterade dödsfall följer Italiens.
Jag har visat er grafer, här är den viktigaste Sverige måste se, vilket jämför med Sydkorea. Observera att Singapore, Hong-Kong och Taiwan hade varit än lägre, och omöjligt att se med blotta ögat.
Dessa länder med nära hundra miljoner invånare har haft Corona i nära tre månader och ingen karantän, men sammanlagd färre inrapporterade dödsfall än Sverige senaste tre dagar. Låt det sjunka in.
Det finns inga tecken på en ny massiv utbrott, kan man stabilt sänka R0 under 1 en gång kan man göra det igen. Orsaken är att de följer motsatt strategi än Sverige, suppression där smittan isoleras med teknik som test/spårning/mask till vaccin. Strategin anses vara best-practice enligt WHO, och är vad Norge, Finland, Tyskland, USA, UK mfl. satsat på.
Ingen måste själv vara virolog för att läsa internationell media och lyssna på experterna över myter.
1. "Alternativet är karantän i två år"
Nej, alternativet är en kort lockdown tills vi har rustat vården och satt upp isolering med teknologi, och kan återöppna
2. "Alla länder följer samma strategi"
Galet, central parameter är smittade, Sverige accepterar ca 50% medan andra vill begränsa & invänta vaccin
3. "Vi kan omöjligen veta förrän två år"
Experterna vet massor redan, inte minst parametrar att tidigt utvärdera strategier, som pålästa medborgare kan sätta sig in.
4. "Det Sydkorea gjorde är omöjligt för Väst att kopiera"
Varför försöker då så många göra det? Tyskland har redan mer testkapacitet än Sydkorea då. Världen producerar 1.5 miljarder smartphones per år, såklart kan man producera miljoner tester med beprövad strategi
5. "Överdrifter, Corona är som en svår vinterinfluensa"
Nej, det tar bara tid för det att döda, I rika Bergamo dog 4500 mer än normalt år, och Madrid har redan fördubblat begravningar. För Sverige motsvarar det överdödlighet på 40.000, konsistent med Imperials modell som övertygade stora delar av världen.
I traumatiserade Bergamo vid samma fas som Sverige är i nu hånades Corona som hysterisk överdrifter, av många som nu är avlidna eller har sett sina föräldrar avlida.
 R
Rrr30629
Gjest
Torsdagen også...selv om man skulle startet en 14 dagers karantene etter onsdagsturen. Fin gjeng.
For noen duster.."Både tollerne og politiet reagerer sterkt på at mange nordmenn brukte onsdagen på handletur i Sverige."
.. alle vet jo at det er torsdagen man skal gjøre slikt.
Kan bli skikkelig dyre disse onsdagspølsene.
https://www.vg.no/nyheter/i/6jR8L8/harryhandlere-anmeldes-for-brudd-paa-karanteneplikt
https://www.nrk.no/osloogviken/anmelder-grensehandlere-for-brudd-pa-karantenereglene-1.14978745Sist redigert av en moderator:
Synd norske tall ikke er tilgjengelig.LItt nyttig info.
data han presenterer:
1 av 5 syke havner på sykehus. 1 av 4 av disse på intensivavdelingen og 1 av 2 av disse dør.
Skulle man samle slekten med oldemor som sentrum i påsken: oldemor, 3 barn(+3 følge), 9 barnebarn (+ 9 følger) og ca 10 oldebar (+3 ca følge).
det blir ca 40 personer. Alle smittet -> 8 personer på sykehus -> 2 på intensiv -> 1 død. i snitt.
1 av 5 smittede på sykehus er spinnvilt mange.
Det er selvsagt mulig å stramme til igjen senere, men med en tidsforsinkelse på to uker eller så blir det fort ganske stygt hvis det først går ut av kontroll, og da kan det bli vanskelig å stappe ånden tilbake på flasken igjen. Det er risikosport å la en gressbrann få spre seg sånn passe mye ut fra en antagelse om at man sikker vil være i stand til å slokke den senere. UK var kanskje det landet som tydeligst satset på "flokkimmunitet", dvs å sitte stille og la viruset spre seg som det ville, men det gikk jo ikke så veldig bra. Når man dro i nødbremsen var det allerede ute av kontroll.Mener du at denne strategien ikke åpner for å innføre strengere tiltak underveis dersom belastningen nærmer seg maks, eller mener du at vi ikke greier å få ned R til 1 eller under - hvis vi først har sluppet det opp så mye..?
https://direkte.vg.no/coronaviruset/news/5e8f2a33474b050011b80242
Danmark har så vidt jeg kan se strengere restriksjoner enn Norge, så det har kanskje ikke så mye å si hva man kaller det. Fra linken:
Ofte nevnes to strategier – den ene er å stanse utbruddet og den andre å bremse utbruddet
(se kapittel 9.1). Flere land vurderer nå at å skille mellom disse strategiene er mindre
relevant, og at strategi og tiltak heller må utvikles og justeres fortløpende basert på ny
kunnskap om sykdommen og utbruddets utvikling, effekt av tiltak og muligheter for bedre
diagnostikk, behandling og potensiale for vaksine. Både Danmark, Sverige og Finland
følger en slik strategi selv om tiltakene de har iverksatt varierer.6 Flere land skiller ikke mellom dette, men har som strategi å iverksette tiltak slik at helsetjenesten har
kapasitet til å håndtere pasientene som får alvorlig sykdom og må behandles i sykehusInternasjonalt legges det nå mindre vekt på å skille strategiene; begge innebærer en
betydelig demping av smittespredningen med hardt smittevernarbeid.Sist redigert:
Dette viruset viser oss forskjeller på helsen blant befolkningen i mange land. Jeg kan ikke skjønne annet, basert på all informasjon statistikk og tall hittil, at vi har betydelig bedre helse i Norge enn både England, Italia og Spania.
Synd norske tall ikke er tilgjengelig.LItt nyttig info.
data han presenterer:
1 av 5 syke havner på sykehus. 1 av 4 av disse på intensivavdelingen og 1 av 2 av disse dør.
Skulle man samle slekten med oldemor som sentrum i påsken: oldemor, 3 barn(+3 følge), 9 barnebarn (+ 9 følger) og ca 10 oldebar (+3 ca følge).
det blir ca 40 personer. Alle smittet -> 8 personer på sykehus -> 2 på intensiv -> 1 død. i snitt.
1 av 5 smittede på sykehus er spinnvilt mange. -
Laster inn…
Diskusjonstråd Se tråd i gallerivisning
-
-
Laster inn…