Dette er interessante saker.
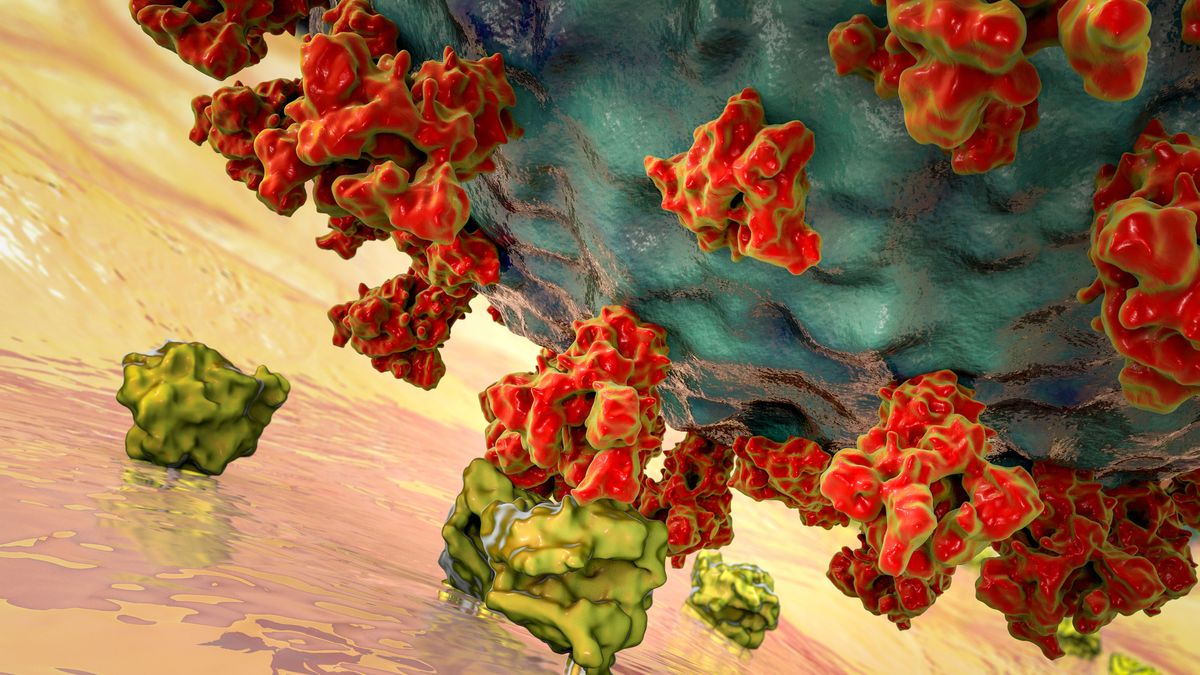
The novel coronavirus causing COVID-19 seems to hit some people harder than others, with some people experiencing just mild symptoms and others being hospitalized and requiring ventilation. Here's why.

www.livescience.com
Bl.a.
Blood type seems to be a predictor of how susceptible a person is to contracting SARS-CoV-2, though scientists haven't found a link between blood type per se and severity of disease.
Jiao Zhao, of The Southern University of Science and Technology, Shenzhen, and colleagues looked at blood types of 2,173 patients with COVID-19 in three hospitals in Wuhan, China, as well as
blood types of more than 23,000 non-COVID-19 individuals in Wuhan and Shenzhen. They found that individuals with blood types in the A group (A-positive, A-negative and AB-positive, AB-negative) were at a higher risk of contracting the disease compared with non-A-group types. People with O blood types (O-negative and O-positive) had a lower risk of getting the infection compared with non-O blood types, the scientists wrote in the preprint database
medRxiv on March 27; the study has yet to be reviewed by peers in the field.
Many medical conditions can worsen the symptoms of COVID-19, but why do historically healthy people sometimes fall dangerously ill or die from the virus? Scientists suspect that certain genetic factors may leave some people especially susceptible to the disease, and
many research groups aim to pinpoint exactly where those vulnerabilities lie in our genetic code.
In one scenario, the genes that instruct cells to build ACE2 receptors may differ between people who contract severe infections and those who hardly develop any symptoms at all,
Science magazine reported. Alternatively, differences may lie in genes that help rally the immune system against invasive pathogens,
according to a recent Live Science report.
For instance, a study published April 17 in the
Journal of Virology suggests that specific combinations of
human leukocyte antigen (HLA) genes, which train immune cells to recognize germs, may be protective against SARS-CoV-2, while other combinations leave the body open to attack. HLAs represent just one cog in our immune system machinery, though, so their relative influence over COVID-19 infection remains unclear. Additionally, the Journal of Virology study only used computer models to simulate HLA activity against the coronavirus; clinical and genetic data from COVID-19 patients would be needed to flesh out the role of HLAs in real-life immune responses.